Papua New Guinea’s TB Crisis
November 29, 2018 | Expert Insights

Papua New Guinea has launched systematic screening for tuberculosis fight a TB epidemic. The government has been criticised for failing to prioritise public healthcare.
Background
Papua New Guinea occupies the eastern half of the island of New Guinea and its offshore islands in Melanesia, a region of the southwestern Pacific Ocean north of Australia. Papua New Guinea is classified as a developing economy by the International Monetary Fund. Strong growth in Papua New Guinea's mining and resource sector led to the country becoming the sixth-fastest-growing economy in the world in 2011. Mining remains a major economic factor in the country. Tuberculosis (TB) is a significant problem in the mining industry. TB rates within the mining workforce are estimated at 2,500-3,000 cases per 100,000 individuals. This incidence is 10 times the WHO threshold for a health emergency and is also nearly three times the incidence rate in the general population.
Tuberculosis (TB) is caused by bacteria (Mycobacterium tuberculosis) that most often affect the lungs. The disease is curable and preventable but remains one of the top 10 causes of death worldwide. An estimated 54 million lives were saved through TB diagnosis and treatment between 2000 and 2017.
Multidrug-resistant TB (MDR-TB) remains a public health crisis and a health security threat. WHO estimates that there were 558 000 new cases with resistance to rifampicin, which is the most effective first-line drug.
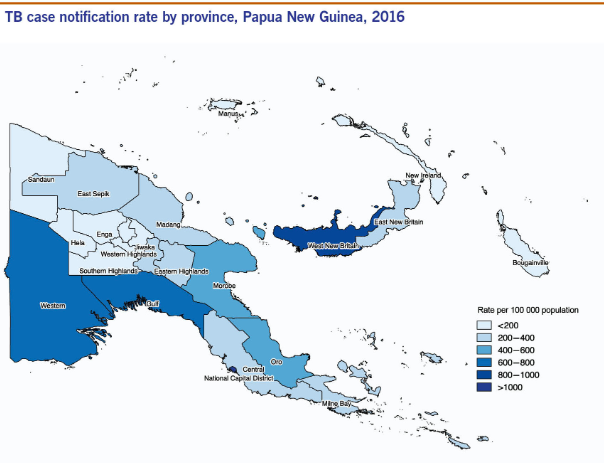
TB is a leading killer of HIV-positive people, and Papua New Guinea has the highest incidence of HIV and AIDS in the Pacific region. The country is the fourth in the Asia Pacific region to fit the criteria for a generalised HIV/AIDS epidemic. Papua New Guinea is one of the 10 highest tuberculosis-burdened countries globally, according to the World Health Organization (WHO). Daru, the capital of the Western Province of PNG, has been declared a global hotspot for the disease by the World Bank.
Analysis
Concerns are growing about the spread of tuberculosis in Papua New Guinea (PNG), where more than one in 250 people are believed to have been infected by the disease.
Providing treatment for the curable bacterial infection that most often affects the lungs, also known as TB, is especially hard in rural PNG, where access and transport to medical facilities is a major issue. Those infected have to take a personalised heavy cocktail of medicine at set times for several months, which poses a major challenge for those living far from health centres.
A significant number of patients are not able to continue their treatment until the end, which in turn leads to TB developing resistance against medication. After being morphed into what is called multidrug-resistant TB, the disease becomes much harder and more expensive to treat, with about half of those infected with this version dying. The WHO estimates that one in 10 TB cases in the area is multidrug resistant, leading to about 500 new cases every year, or about three per cent of the city's population.
Counterpoint
The country's government has come under fire for the way it has tried to combat the epidemic, even though the funds to contain it are available.
Critics have pointed to PNG spending millions of dollars on hosting the Asia-Pacific Economic Cooperation (APEC) conference earlier in November as an example of how the government has its priorities out of order.
Deputy Prime Minister Charle Able recognises there have been issues with the treatment of patients. "While money for medicines has been there in quite a large number, it has been the execution of the health services at the front end that has suffered. Our government has tried to emphasise that some of the funding streams are essential for the delivery of those services.”
Papua New Guinea has launched systematic screening for tuberculosis in Daru Island in the Western Province with everyone 10 years of age and older being checked for the deadly disease. Health workers will screen for all types of tuberculosis, including drug-resistant strains that threaten the effectiveness of standard TB remedies.
Assessment
Our assessment is that the systematic population screening programme if executed correctly, could be tremendously beneficial to Papua New Guinea’s tuberculosis epidemic. We believe that earlier diagnosis through screening will help strengthen the TB response and lead to better outcomes for patients, in addition to stopping the disease being transmitted.
In our opinion, a partnership between the National Department of Health and other stakeholders, as well as a strong community response, are crucial to progress.
India Watch
Worldwide India has the highest burden of both TB and MDR TB. India also has the second highest number of estimated HIV associated TB cases.
2.8 million people developed TB in India in 2015, accounting for 27% of the global instances of the disease. 0.13 million people in India developed multidrug-resistant or rifampicin resistant tuberculosis in India in that year. In March 2017, the Government of India announced that the new aim with regard to TB in India was the elimination of TB by 2025. TB treatment and care in India is provided in the public sector by the government’s Revised National TB Control Programme (RNTCP) as well as through private sector health providers. The RNTCP is responsible for implementing the GoI’s five-year plan to combat TB.







Comments