A Gut Feeling?
February 10, 2024 | Expert Insights

Gut microbes (bacteria and other microorganisms) could offer a critical link between the digestive tract and how we feel. A century back, a few scattered studies had pointed to this link.
More recently, this concept has resurged, and it is now emerging that gut health may contribute to mental health as the gut-brain connection becomes a vibrant topic of interest.
Background
In the early 20th century, an English doctor in London, Dr. George Porter Phillips, observed that his patients with melancholia often experienced constipation and other signs of blocked metabolic processes. While most people would have assumed that depression could cause those physiological issues, Phillips wondered if it went the other way around. Could the gut offer solutions to melancholia?
He altered their diets, cutting out all meats except fish and adding a fermented milk drink called kefir containing the "friendly" lactobacillus bacteria that ease digestion. To his astonishment, it worked on 11 of the 18 patients and substantially improved two others.
Despite early studies, the possibility that the gut could influence mental health was discarded for most of the 20th century. It is only recently that a renewed interest in this unexpected link has emerged along with strong evidence over the last couple of decades.
A leading experiment in Japan in 2004 showed that mice raised in sterilized conditions so that they had no microbes displayed higher fluctuations in the hormones that reflect stress levels. Further, mice that receive the "depressed" microbiome (community of microbes) showed signs of depressive behaviour. In another study, a sample of gut microbiota was transferred from human patients with Major Depressive Disorder to mice. These mice went on to exhibit behaviour associated with depression, such as quitting a task sooner.
These animal studies are corroborated by human studies showing that differences in gut microbiota are associated with mental health conditions like depression and anxiety. Gut microbes have even been linked to brain-based disorders like autism and Alzheimer's.
Analysis
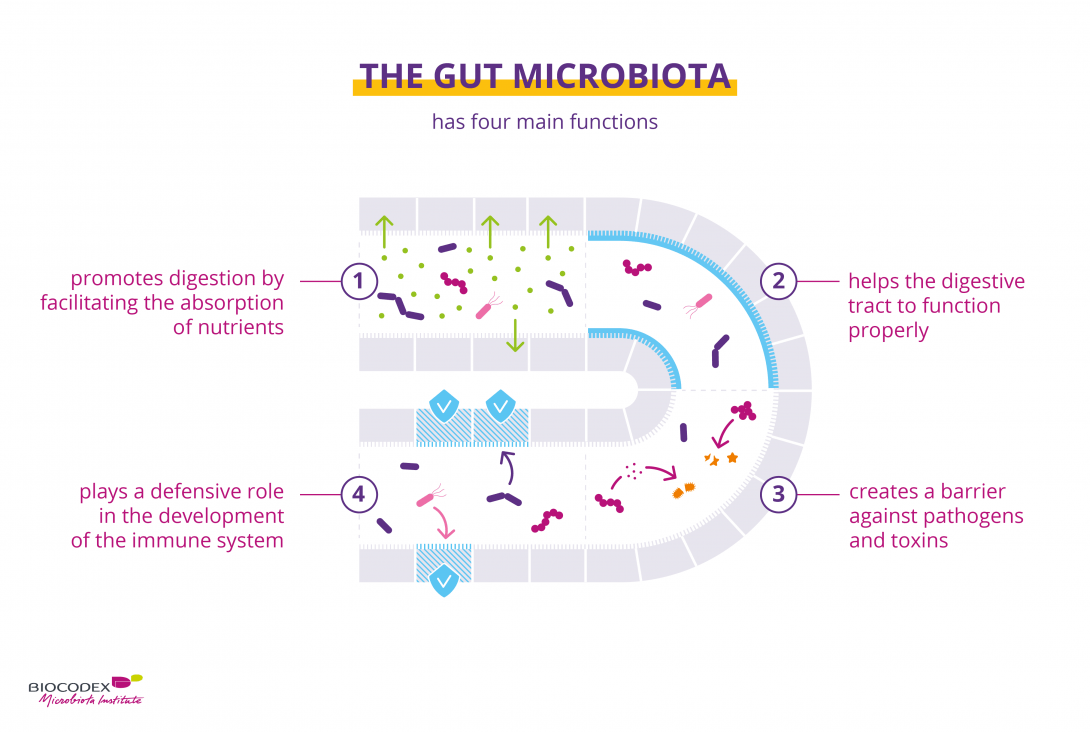
The digestive system walls contain about 100 million nerve cells, collectively called the enteric nervous system. Recent advances have uncovered a two-way communication between the brain and gut, known as the gut-brain axis, linking the emotional and cognitive centres of the brain with the digestive tract. While the brain’s effect on the gut may be easier to understand, the gut’s effect on the brain and mental health is still being unveiled.
In a preventive way, certain gut microbes protect the gut wall and prevent its contents from spilling into the bloodstream through the mucous barrier in what is known as a "leaky gut", which also leads to a low mood and lethargy.
More significantly, gut microbes are key in digesting and metabolizing substances that form important neurotransmitters like serotonin and dopamine. The intestine produces most of the body's serotonin through specialized cells in its walls, which release serotonin when stimulated by food, which then acts on nerves that signal the brain. Serotonin is a chemical used in antidepressant drugs and is believed to contribute to stabilizing the mood.
Additionally, the vagus nerve, a critical parasympathetic nerve controlling functions like heart rate, digestion, mood and more, directly connects the gut lining to the brain. Since its receptors tap into the digestive tract, intestine microbes can release chemical messengers that affect the vagus nerve’s signalling to the brain.
Moreover, studies have found that probiotics enhance the effectiveness of antidepressant treatments. Probiotics are live microbes that can help the body maintain or revive a healthy flora of microorganisms. They are present in fermented foods and are also offered as diet supplements.
The exact mechanisms of the gut-brain axis are still being uncovered. As more understanding emerges, particularly in terms of specific “good” bacteria and their effects on mental health, it may be possible to come up with targeted treatments for conditions like depression.
Assessment
- Gut health, particularly a flourishing flora of healthy bacteria, could significantly contribute to mental health and wellbeing. Whether it's the gut's role in producing neurotransmitters affecting the mood, its nerve communications with the brain, or the strange benefits that probiotics seem to have in treating depression, "friendly" microbes seem to contribute to emotional stability.
- While the specifics of the gut-brain connection are still being uncovered, the gut could open up a range of potential treatments such as specific bacteria being used to treat mental health conditions in a targeted way.








Comments